Help, I can't see my appointments!
Screenshot once you’ve logged in to your account.
Help, I can’t see my appointments!
Can’t see your appointments? You are not alone, but rest assured they are there!
It’s a fact. Patients love the ability to schedule their appointments online. “It’s a great service.” The technology makes it easy for patients but also possible for small, privately owned healthcare practices to operate like a fully staffed front office. But, occasionally, an update to a platform can change how things look on both the business and patient end. This happened recently with our scheduling platform.
At first glance, it looks as though you may not have any appointments because the format has changed. Rest assured, your appointments are still there! The changes are not intuitive, so let us help you.
Follow these steps to see your scheduled appointments
Log into your account.
Locate your username/email. See the photo above.
Click the arrow next to your email address. A drop-down menu will appear. See the photo below.
Click on “Appointments.” You should be able to see all your upcoming and past appointments.
Still having trouble?
Please get in touch with Allison if you still can’t see your appointments.
Announcing a Podcast Hosted by Coach Amy with her Coach, Liz.
Cool looking album art.
Introducing a Podcast
Should you use ice or heat to treat an injury or for post-run recovery? How about a massage gun? What is recovery?
We answer these questions and more on The Coach Amy and Coach Liz Show, a podcast for endurance athletes from the perspective of two coaches, two athletes, and a physical therapist. And in the process, we share our experiences as athletes and patients - the good, the bad, and the ugly.
Not an endurance athlete? That’s okay; most active people will find many topics relevant.
Listen and Follow
The podcast goes live with the first three episodes on Sept. 20th. Until then, listen to the teaser trailer in iTunes or Spotify and follow us wherever you get your podcasts.
Learn More
Visit our podcast landing page to learn more.
We are in this Together
Recommend us! Promote a healthy and positive experience in endurance sports by helping other endurance athletes discover this podcast. Not sure how? In the podcast trailer, click on the (…) and choose share.
Can I Run During an Injury and if not, When can I Return to Running After Injury or Surgery?
These are million-dollar questions! My answer is, "It depends."
A patient with patellar tendonitis, whom I instructed not to run, came into his appointment and said, "I feel great, and I ran seven miles two times last week." I lifted my head from my laptop, peered at him through my glasses, and gave him a grin and head nod of understanding while at the same time resisting the urge to roll my eyes back in my head.
As a runner who has experienced many injuries and surgeries, I empathized personally, but as a physical therapist, it is cringeworthy when a patient goes rogue.
Why rest from running or manage your return to running after an injury or surgery?
The musculoskeletal system, which includes bone, takes time to heal and strengthen progressively. When running, the structures must tolerate repetitively loading at least three times your body weight.
Several factors determine whether you can run during an injury or when you can return to running after an injury or surgery.
When and whether or not you should run depends on an injury's nature, severity, and chronicity. Does the injury involve bone or soft tissue like a tendon? Is the injury mild or severe? How long has it been present? Six months, three years, or two weeks?
Nature of the injury or Surgery.
If the injury involves tendons and ligaments, it can sometimes take longer than a fracture to heal. The rule of thumb for tissue repair is at least six weeks if you do all the right things! Some surgeries require six weeks of rest from running and high-impact sports, and others require six months or more. Runners undergoing surgery should always have post-operative physical therapy if they want to return to sport.
Severity of an Injury.
The more severe the injury, the longer it will take to return to running. For example, a grade III calf injury may need months of rest, while a grade I calf injury may only require a week of rest from running. Check out my article on Calf Strain and Pain.
Chronicity of an injury.
The longer an injury has festered, the longer it will take to return to running. This is a rule of thumb, and I find it is usually accurate. And why all runners should seek professional help if an injury does not subside within a week of rest and modification.
Signs, symptoms, and issues that indicate you need to rest from running or wait to return to running after an injury or surgery.
Poor biomechanics due to lack of stability, strength, or range of motion
Swelling/inflammation
Pain greater than a 3/10 during or after running
Poor Biomechanics
Many runners can feel when their run gait is “off” or when weakness or lack of mobility is present. Weakness and/or loss of range of motion is your body’s way of telling you that something is off - they are protective mechanisms. Pushing through a run in these circumstances will delay healing, worsen the injury, or even cause another injury!
Swelling and Inflammation
Swelling is a sign that the body is not okay. It is a red flag, a warning to stop running. Intermittent, mild swelling may be permitted with a return to run, but it means that you’ve done too much. Ensure you are working with a physical therapist to help you manage your back to run the program. Check out my article on Aiding and Controlling Inflammation.
Pain
Once again, it is a warning sign that something is not right. If unmedicated, your pain is greater than a 3/10 on a pain scale where 0 is no pain, and 10 is emergency room pain, then you should not run. Do not take pain medication to run. Pain is a fascinating and multi-faceted topic, and your physical therapist can help you navigate when it is okay to have some pain. Check out my article: Pain and Injury Doesn’t Mean You Have to Quit.
Resting from running impacts our mental health. Acknowledging and addressing our mental headspace is just as important.
Following my patient’s admission to running, an explanation ensued, "I don't drink, I don't smoke, and I don't do drugs. I run." Running releases serotonin, which makes us feel good, and it is a mental escape, a muse. Taking it away from us for too long can mess with us physically, emotionally, and mentally. Fear of losing fitness comes at a close second to the effect on our headspace.
Acknowledge this aspect and work with your physical therapist to manage it with modifications and alternatives for running.
Modifications in running during injury and returning to running programs after injury are not one size fits all! It is personal and individual.
With mild injuries, sometimes running can continue, albeit modified in volume, intensity, and perhaps surface, while you heal. When it comes to a back-to-run program or continuing to run while managing an injury, finding the right recipe can be complicated: it takes practice, finesse, and patience. It's an art as much as a science, and an experienced physical therapist specializing in running can help.
Your physical therapist will continually test you to ensure you meet benchmarks for return to run and, when you meet them, will set you up with a back-to-run protocol. That protocol will consider how much time you’ve rested from running, your specific injury or surgery, your running experience, and your tolerance.
Invest in your running future.
My patellar tendonitis patient was lucky. Most runners that do this rouge testing don't fare as well and end up setting back their healing and their return to run. Pay attention to the signs and symptoms that should stop your run, and seek professional help for managing your rest, modification from, and return to run; it is an investment in your running future!
Stop injuries before they occur!
Learn the top five training errors that lead to injuries in runners in this blog post.
How to treat Delayed Onset Muscle Soreness
You know that feeling of sore muscles after a strenuous strength workout? There is a name for that! It’s called DOMS, and Coach Amy has some advice for what to do when this happens.
What is DOMS?
Delayed Onset Muscle Soreness (DOMS) occurs 12-24 hours after a workout. It is okay and normal to experience mild-moderate cases of DOMS, especially with certain kinds of exercises. Do not confuse DOMS with pain due to injury, which occurs almost immediately. If you suspect an injury, click on the button below.
How do I treat DOMS?
Resting the affected muscle groups, dynamic movement, and cross-training are the best medicine in mild to moderate cases.
DOMS Treatment List
relative rest
dynamic mobility
moist heat
compression socks/sleeve
Kinesio Tape (applied for lymph drainage)
cupping
light massage/myofascial release
proper hydration and nutrition
Reduce the intensity and duration of exercise for 1-2 days following intense DOMS-inducing exercise. Resting the areas of the body experiencing DOMS allows proper recovery so you can resume training quicker. You can exercise less affected body parts during this time and perform gentle dynamic movement of affected areas.
In severe cases of DOMS, Tylenol can help with pain. It is not an anti-inflammatory. Taking Tylenol with certain prescription medications or in the case of certain medical conditions can be contraindicated. Always check with your doctor first if you are uncertain.
What NOT to do when experiencing DOMS.
Successful training relies on a normal inflammatory repair process. If you hamper that inflammatory process with ice and NSAIDs, you could negatively impact your overall training response. Deep tissue treatments and stretching during early DOMS can also delay healing and cause injury.
During the DOMS, avoid the following:
stretching
NSAIDs (non steroidal anti-inflammatories e.g. ibuprofen)
Ice and ice baths
deep tissue massage
percussion massage
deep tissue treatment devices like scrapers, dense foam rollers
If you do not recover from DOMS within 24 hours of onset, talk to your physical therapist, coach, or personal trainer so they can help you modify and navigate the recovery process successfully.
DOMS happens. Honor it and know what to do so you can resume training safely.
Massage Guns: Do or Don't?
"Should I use a percussion device or massage gun?"
That is an excellent question; unfortunately, many patients and athletes assume devices they see at race expos, post-race recovery tents, or in magazine articles are safe and don't question it.
My answer is no; you should not use a percussive device or massage gun. Before you discard yours or ignore my answer and go ahead and use it anyway - yes, I know who you are - please hear me out.
The reason I do not recommend the use of percussive devices or massage guns is that the risks outweigh the benefits. Unlike vibrating massage heads or foam rollers, these devices create a downward force into the body's tissue like a jackhammer, and the smaller the head(s), the more concentrated the power. This hammering force can cause damage, sometimes severe.
Unfortunately, athletes, in particular, associate "pain" with stretching or massage as beneficial. "It hurts, so it must be working." That is rarely the case. It is difficult for injured or sore athletes to discern when it is acceptable to feel discomfort with a self-treatment method like a massage gun.
Risks of using a massage gun
Safely using a percussive or massage gun requires a thorough command of human anatomy. Besides a general knowledge of where the claves, glutes, and hamstrings reside, most athletes and patients are unaware of the location of nerves, blood vessels, lymph nodes, bursae, organs, tendons, or ligaments. Improper device placement over these structures can cause severe damage.
Massage guns on injured and inflamed connective tissue can further damage the structure and increase inflammation. For example, use on a torn ligament, like an ankle sprain, could injure it further.
There are many examples of patients in my clinic who improperly used a massage gun to treat their soreness, pain, or injury. Below are four cases.
Case #1
A patient attempted to treat his groin pain, in this case, psoas tendonitis, and placed the gun in the area where the femoral nerve, artery, and vein reside. Not only is it contraindicated to use the device on the injured, inflamed psoas tendon, but the risk for vessel and nerve damage was high in this area.
Case #2
A patient tried to treat his pectoral muscle strain and aimed the device in his armpit on a large bundle of nerves called the brachial plexus. Damage to these nerves could cause temporary or permanent disability to the entire arm/hand.
Case #3
A patient attempted to treat her knee pain and aimed the device at the painful spot but didn't realize that what "hurt so good" was the peroneal nerve. Damage to this nerve could cause foot drop - or lack of the ability to lift the foot.
Case #4
A patient tried to treat her sore "glute" with the massage gun but didn't realize she aimed it at a bursa (a fluid-like sack) in the same area. Because this was my initial visit with her, it is hard to know if she was suffering from bursitis before using the gun or afterward, but in either case, her injury and pain were worse.
Dangers and contraindications for massage gun use
While rare, a percussive massage tool can sometimes cause severe or life-threatening injuries, including fractures or joint damage, deep vein thrombosis, and rhabdomyolysis.
Using a percussive massage gun can cause a fracture in persons with osteopenia or osteoporosis. Never use a massage gun at the site of a fracture - even a stress fracture. If you suspect a fracture go to the emergency room or an orthopedic urgent care center.
Deep vein thrombosis is a rare but life-threatening condition, especially for post-surgical patients. It tends to show up as calf pain and soreness. A massage gun on that sore calf could dislodge the blood clot and cause a pulmonary embolism and death. If you are experiencing symptoms consistent with a blood clot, go to the emergency room.
Rhabdomyolysis is a severe and potentially life-threatening condition. Endurance sports athletes are particularly at risk of acute exercise-induced rhabdomyolysis (AER), which can occur after profound overexertion, such as after a long run, ride, or race. Endurance athletes using percussion massage to treat delayed onset muscle soreness after an endurance event or training session may be at a higher risk.
There is a case in the literature of a patient who suffered a case of severe rhabdomyolysis after percussion massage: Chen, J., Zhang, F., Chen, H., & Pan, H. (2021). Rhabdomyolysis After the Use of Percussion Massage Gun: A Case Report. Physical Therapy, 101(1). https://doi.org/10.1093/ptj/pzaa199
Not ready to throw your massage gun in the trash?
Limited research supports that a percussion device can help with increased mobility when used on healthy tissue and when operated by a healthcare professional. The risks outweigh the benefits, but if patients and athletes insist on using them, I recommend scheduling an appointment with a physical therapist to learn how to use them safely.
While your health is serious business, we can also take a minute to laugh about the massage gun. Check out comedian Tom Papa’s bit about these “weapons-grade jackhammer massage guns.” Tom Papa: What A Day!
Alternatives to achieve mobility
Physical therapists, patients, and athletes have many safer alternatives to achieve mobility. Subscribe to Coach Amy Says to receive upcoming posts on how to achieve mobility and why Coach Amy does not recommend stretching as well as other tips on injury prevention, wellness, and performance.
Coach Amy discusses massage guns and all things endurance sport with Coach Liz in their podcast, The Coach Amy and Coach Liz Show. Coming soon to Apple Podcasts, Google Podcasts, and Spotify.
Treating Migraines with Neurological Dry Needling
What is a migraine, and what causes them?
Migraine headaches are a genetic neurological disease. Multiple factors can trigger migraines, such as hormones, stress, lack of sleep, alcohol, caffeine, food allergies, overuse of medications, smell, light, and dehydration.
Injury to the neck muscles, joints, and nerves can cause migraine-like symptoms and trigger a migraine in sensitive individuals. We refer to problems with this area of the body as cervicogenic.
What is a cervicogenic headache?
Cervicogenic issues may arise from a sports injury, whiplash, arthritis, pinched nerve, muscle strain, or poor posture.
Dry needling can treat most cervicogenic headaches and help individuals with the migraine headaches they trigger.
How does neurological dry needling help treat headaches?
Studies show that the trigeminal nerve is overstimulated and inflamed in cervicogenic and migraine headaches. Integrative Dry Needling System (IDNS) techniques can help reduce the inflammation of this nerve and its many branches, thereby decreasing the frequency and intensity of migraine headaches.
How can Coach Amy help you with your headaches?
Coach Amy is certified in IDNS. She treats the neuromuscular and biomechanical causes of both types of headaches with the following:
patient education
dry needling
manual therapy techniques like active release
joint mobilization
posture and biomechanics training
“After the first treatment, the results were life-changing. For six months I had woken up with a headache, but these immediately disappeared. For over a year, I often canceled plans because I could not leave home, but now I can plan because I know I won’t be stuck in bed with a headache. In the past five months, I have only had 3-4 migraines, which are less severe. Dry needling with Coach Amy has been central to my recovery.”
While dry needling will not cure migraine headaches, it may help decrease the frequency and intensity, especially those triggered by cervicogenic issues.
Schedule an appointment with Coach Amy to evaluate if neurological dry needling and physical therapy can help minimize your migraines and improve your quality of life.
The Science Behind High-Intensity Laser Therapy (HILT)
How does high-intensity laser therapy (HILT) help heal various musculoskeletal injuries?
Remember introductory high school science class? Does photosynthesis ring a bell? How about mitochondria and ATP? These concepts are foundational in understanding the science behind HILT. But don't worry if you don't remember! I will explain.
Boosts Cellular Energy
When your body is recovering from an injury, the cells (e.g., muscles and nerves) require energy to build and repair. HILT boosts that cellular energy and activity.
Let's take out a virtual microscope and zoom in on a slice of quadriceps (thigh) muscle. Zoom in further; you will see bundles of skeletal muscle cells that comprise the thigh muscle. Zoom in once more, and inside those muscle cells are mitochondria. These are kidney bean-shaped organelles responsible for creating energy (ATP). See the drawing above.
HILT penetrates the skin and travels deep into the quadricep muscle cells. It stimulates their mitochondria to generate more ATP (energy), so the cell can be more active, allowing them to create the building blocks that repair the muscle; this is just an example of a muscle cell. HILT also increases energy production in other connective tissue cells, including nerves, ligaments, and tendons, in the same way.
Aids in the Transport of Nutrients
Cellular repair requires energy, but we also want to remove waste products caused by the injury and bring needed nutrients to the area so the cells can build new, healthy tissue. HILT dilates blood vessels, increasing blood supply which transports nutrients required for cellular repair, and removes waste products released by the injured tissue.
Enhances Cellular Mobility
Injuries, disease processes, and conditions like frozen shoulder and, often, surgery cause scar tissue to develop; tissue fibers become cross-linked and stiff, interfering with mobility and, ultimately, function. HILT helps release the cross-linked fibers. The result? Muscle, capsular, and ligament relaxation.
HILT is one treatment method and does not stand alone.
HILT is a powerful addition to a well-rounded arsenal of treatment methods, such as manual therapy, dry needling, and applied functional exercises—along with Coach Amy's ongoing evaluation methods based on principles of biomechanics. No treatment offers an effective long-term solution without pinpointing the root cause.
Do you have more questions about HILT?
High-Intensity Laser Therapy FAQs cover everything from what to expect during treatment, how many sessions you may need, how to prepare, and more.
Coach Amy breaks down what HILT is and isn’t in this article: Introducing High-Intensity Laser Therapy at CoachAmyPT.
HILT helps treat conditions from head to toe, including pain syndromes, nerve and joint problems, and muscle and tendon damage. Coach Amy will explain it in an upcoming article: Conditions HILT Helps Treat.
High-Intensity Laser Therapy - FAQs
image from high-intensity-laser.co.uk
What is HILT?
HILT is a non-invasive and painless treatment method. It stimulates cells, including pain receptors and the immune system, and can increase blood flow and decrease pain. It promotes the repair of damaged tissues of the musculoskeletal system and nerves, which can help with neurological regeneration. Stay tuned for Coach Amy’s article: The Science Behind HILT - How Does It Work?
What conditions does HILT treat?
HILT is a treatment, not a cure; it is supplemental to other physical therapy methods such as manual treatment, dry needling, biomechanics, and functional exercises. It is not a stand-alone treatment. It helps in the treatment of:
Neuropathy and neuromas, nerve entrapment, carpal tunnel syndrome
Fascitis
Musculoskeletal injuries (tears, bursitis, fractures, sprains/strains)
Tendonitis/tendonosis
Back and neck pain (herniated disc, facet joint syndrome)
Joint pain
Frozen shoulder
TMJD
Rotator cuff injuries/impingement syndromes
Pain syndromes (fibromyalgia)
Headaches (tension, cervicogenic, migraines)
Arthritis (osteoarthritis and rheumatoid arthritis)
This list is not all-inclusive. Ask Coach Amy if HILT will help with your specific condition.
How many treatment sessions will I need?
The number of sessions depends on the nature and duration of your condition and other factors. Some acute conditions will respond in 4 or fewer sessions, whereas chronic conditions may take several more treatments. You can expect some progress and change within 1-4 sessions. When a patient does not demonstrate progress after 3-4 treatments of HILT, Coach Amy re-evaluates the diagnosis and treatment protocol.
Some chronic conditions require ongoing care, e.g., 1/mo—tune-up sessions to sustain pain relief and functionality. Coach Amy will discuss your personalized plan of care with you.
How much does treatment cost?
The quotes below are effective 3/2024. Prices are subject to change.
Self-Pay Patients
Coach Amy can incorporate HILT into a regular appointment. The total price of Self-Pay with HILT add-on is $180.00.
Blue KC Patients
BCBS does not cover HILT. Coach Amy can incorporate it into a regular PT appointment at an additional cost of $70.00. You are also responsible for the copay or coinsurance due for covered services provided during the treatment session.
For more information on the cost of physical therapy, see FAQ: How much does physical therapy cost?
Can I book a laser-only treatment?
15-minute follow-up HILT costs $80.00 and is for established patients only on a case-by-case basis. These appointments require an initial evaluation within the treatment year and 1/mo. 40 min—appointments for supplemental treatments and reassessment. Please email Coach Amy before booking if you are unsure.
What does HILT feel like?
Most patients describe it as a very soothing, warm sensation. Because it is a high-powered laser, your skin will get warm during the treatment. Many patients feel a significant reduction in pain on the first visit. Occasionally, patients will feel slightly more pain immediately after the treatment but feel much better the next day.
How will I feel after the treatment?
You may feel pain relief after the first treatment. For some patients, it takes a while longer. Most patients report feeling very relaxed or even tired.
I feel a lot better- but Coach Amy prescribed more than one session of HILT. What should I do?
If you experience a reduction in pain, remember that pain reduction is just one goal. HILT boosts cell energy, so they repair and regenerate new tissues, which takes time and successive treatment. HILT is cumulative and requires dosing similar to a round of medication. See above: "How many treatment sessions do I need?"
Do I need to take special precautions after HILT?
One effect of HILT is vasodilation, which increases blood flow and lymph drainage; this helps reduce inflammation but can cause soreness. You can soak in EPSOM salts, moist heat, or apply soothing cream to the area.
Why must I wear safety glasses during the treatment?
HILT is a high-powered laser. The lens of your eye can focus class IV laser light and potentially cause damage to your retina. The safety glasses block out the damaging wavelengths of light.
Is HILT safe?
HILT is safe if administered by a trained physical therapist. Coach Amy is trained and certified to use a safe and effective FDA-approved Therapeutic Class IV laser to stimulate cellular repair and decrease pain.
High-intensity laser therapy (HILT) emits powerful beams to quickly provide a desired high amount of multi-directional energy to deep tissues. The laser is applied in long smooth strokes for several minutes to provide adequate dosage levels to structures below skin level, like muscles and nerves.
While the therapeutic laser is a class IV laser, it is not a surgical laser. The therapeutic laser disperses the energy in a broad area for healing purposes, unlike a surgical laser which distributes the power in a concentrated area to cut, coagulate, and evaporate tissue.
Are there any risks to HILT?
HILT is a valuable treatment for musculoskeletal pain and injury; however, there are possible complications like any treatment. While these complications are rare, it is essential to consider them before consenting to therapeutic laser treatment. You must sign a consent form before receiving HILT.
Risks may include mild bruising, temporary increase in pain during the application process and the following day, temporary dizziness, and reaction with photosensitizing drugs (certain antibiotics, for example). Please check with your doctor or pharmacist if you are unsure whether you take a photosensitive medication. Coach Amy maintains a list at the clinic.
Are there contraindications to HILT?
Many of the few contraindications for therapeutic lasers are relative rather than absolute. Caution and consideration for:
pregnancy
history of seizures
growth plates
history of cancer
photosensitizing drugs
radiation therapy
A skilled clinician, together with careful patient selection, should minimize risks.
How do I prepare for a HILT session?
High-powered lasers react with jewelry, dark hair, and lotions. Coach Amy prepares the treatment area to ensure your safety, but you can help by preparing for your session.
Remove jewelry and any reflective clothing.
Wear comfortable, loose-fitting clothing around the treatment area. Laser is applied directly to the skin.
Fill out your consent forms before your first treatment session.
Secure long hair in a hair band if the treatment area is the face or neck.
Do not apply lotions or creams before treatment.
Make sure the treatment area is clean.
I have more questions about HILT.
If you have more questions about HILT, please ask Coach Amy at your next appointment.
Introducing High-Intensity Laser Therapy at CoachAmyPT
image from inmotionpainsolutions.com
Drum roll, please!
After a thorough dive into the efficacy of High-Intensity Laser Therapy (HILT), we are excited to announce that we are adding it to the services provided at CoachAmyPT.
Many of us like to consult Google, friends, and family for medical advice, experiences, and information. Sometimes those sources are helpful; other times, we can fall into a rabbit hole of well-intentioned but incorrect info. We want to ensure your decisions regarding HILT are based on fact.
So, let us get started!
What is HILT, and what isn't?
HILT is a non-invasive and painless treatment method. It stimulates cells, including pain receptors and the immune system, and can increase blood flow and decrease pain. It promotes the repair of damaged tissues of the musculoskeletal system and nerves, which can help with neurological regeneration. Stay tuned for an article, The Science Behind HILT - coming soon.
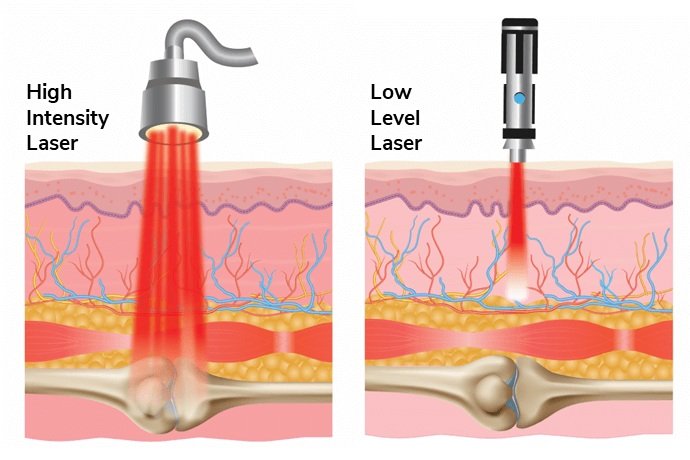
High-Intensity Laser Therapy (HILT) is high-powered and uses a class IV laser, not LED light therapy or cold laser. It is not low-power laser therapy (class IIIb).
The main difference between HILT and low-power laser therapy is that the more powerful beams (power >500 mW) penetrate deeper, bringing a desired high amount of multi-directional energy to deep tissues quickly.
What this means for you:
HILT is more effective and produces results that other light therapies do not.
HILT requires fewer doses than other light therapies and, therefore, less accumulated out-of-pocket expense. e.g., 5-6 treatments v.s. 20 treatments
HILT requires less treatment time: 5-8 min instead of 20-30 min; therefore, the practitioner can employ other complementary treatment methods during the same physical therapy visit.
While the therapeutic laser is a class IV laser, it is not a surgical laser. The therapeutic laser disperses the energy in a broad area for healing purposes, unlike a surgical laser which distributes the power in a concentrated area to cut, coagulate, and evaporate tissue.
High-intensity Laser Therapy is not a stand-alone treatment. It supplements and enhances other physical therapy methods like manual therapy, functional exercises, and addressing the biomechanical cause of an injury.
If Coach Amy determines you may benefit from HILT, she can incorporate it into a regular Self-Pay or BCBS Insurance Physical Therapy appointment at an additional cost.
Coming Soon
Coach Amy is writing several articles to help you learn more about HILT.
Conditions HILT Helps Treat.
HILT helps treat conditions from head to toe, including pain syndromes, nerve and joint problems, and muscle and tendon damage. In this Article, Coach Amy lays it all out.
The Science Behind HILT - How does it work?
Coach Amy takes you back to high school science and explains how HILT works. Don't worry; you will understand it even if you didn’t pass high school science.
Is HILT safe?
Coach Amy is trained and certified to use a safe, effective, FDA-approved Therapeutic Class IV laser. This article outlines the risks, precautions, and contraindications of HILT.
HILT FAQs.
We know you have many questions! This article covers everything from what to expect during treatment, how many sessions you may need, how to prepare, and more.
To receive these articles, subscribe to Coach Amy Says blog. See the button below.
An Interview with Coach Amy
“Once in a while, after a treatment session, I will ask a patient, “how much do I owe you for today?” ”
Coach Amy answers common patient queries about her path into the wide world of healthcare and the physical therapy profession.
Did you always plan to work in healthcare?
No, I was a journalism major, and as a sophomore in college, I realized that career would not fulfill my desire to help people - I didn't feel it would be rewarding for me. So I took a 180 and became a pre-med student. All those journalism and marketing classes went by the wayside, but I retained some communication and writing skills, which have served me well in running a business. Plus, destiny played a role in my career; I remember as a child tending to my neighborhood friends with Bactine and Bandaids in my bathroom "clinic" if they ever sustained even the slightest scrape!
When did you decide to become a Physical Therapist?
I graduated from the University of Kansas as a pre-med student with a major in human biology and a minor in chemistry which I still can't believe because I was not fond of chemistry. But to satisfy the requirements for medical school, I took enough to qualify for a minor.
After graduating, I married and took a gap year before it was commonplace. It was primarily to study for the MCAT, but I also questioned my career path: was it one where I could also raise a family? I was fortunate enough to secure a job as a Physical Therapist Technician or PT Tech during that time. And I liked the profession so much that I ditched the MCAT for the GMAT and applied to PT school. Funnily enough, it was harder to get into PT school than medical school because fewer spots were available then. I remember being notified that I was accepted to the KU Med physical therapy master’s program. I was elated!
Why did you decide to open a private practice?
Starting my physical therapy practice was unplanned; I never envisioned it for myself. But the timing was right in my personal and professional life. With the current state of healthcare creating pressures and pinches on how a physical therapist practices, I thought about retiring but decided to try instead to provide quality care in a way that I was proud of, and it ended up working out! I couldn't have succeeded without the support of my family, friends, and patients, and I am grateful to them every single day. I get to do what I want, how I want, and I treasure that.
How did you choose the specialty of orthopedics and sports injury?
I think it chose me! My plan in physical therapy school was to become a pediatric specialist. However, after one 6-week rotation at Children's Mercy, I realized I didn't have the creative stamina to keep up. Pediatric physical therapists are a unique breed with incredible energy.
Instead, I unceremoniously landed in outpatient orthopedics, where I honed my manual skills while, at the same time, my love of running and endurance sports rekindled. About a decade later, my coach and former KU physical therapy classmate, Steve Hinman, retired and entrusted me with his established running club business, Personal Best Running and Fitness, now Roadrunners of Kansas City. This surprise gift led me down a path I couldn't have imagined. Endurance athletes began to seek me out for coaching and treating their injuries because I understood the sport professionally and personally. I would never have predicted the marriage of my love of running and endurance sports with my professional life. It chose me, and I'm so lucky!
Do you treat conditions and injuries that are not running-related or sports-related?
Oh, yes! I get this question a lot from current patients who want to refer their mother, brother, parent, friend, etc., who has an injury or chronic pain that isn't sport-related. My specialty is treating musculoskeletal injuries, encompassing many issues plaguing nonathletes and athletes. My niche is running and endurance sports, but I relish treating conditions outside that bubble because it provides me a lot of variety.
How can you see problems with running form without taking a video?
I get this question from students of physical therapy. I remember that sense of amazement and frustration as a student and a new grad. I'd watch seasoned physical therapists assessing walking and running gait and couldn't see what they saw; it seemed they were making stuff up. It took lots and lots of practice. It helped to take video at first, so I could rewind, pause and replay. But after a while, picking things out became more natural and easy.
Now, my brain translates what is happening in real time in slow motion. If I were a student reading this, I'd want to punch me in the face, but trust me - it comes with time and lots of consistent practice. Infrequently assessing run gait will not do it. But on the flip side, the more you study it, the more you realize that the science of running gait is a vast universe we have yet to understand fully. So, there is some "winging it," but when you fit the gait assessment in with the other puzzle pieces gleaned from an evaluation, it begins to take enough shape to make informed decisions for a patient. Warning: once you become a seasoned gait assessor, you'll find you can't turn it off; I struggle to ignore it when I run a race or attend a race to cheer!
What is your favorite part of being a physical therapist?
That is a two-parter. First, I like when a problematic case throws me a challenge. I enjoy solving a puzzle no one else has or at least fitting in more of the pieces. In other words, I like when I can help a patient improve who otherwise wasn't.
Second, I enjoy developing relationships and spending time with my patients, which is only possible because I own my practice. In today's healthcare environment, most physical therapists only perform evaluations and monthly reassessments. They don't get the luxury of treating their patients; if they do, they may treat 2-3 patients simultaneously. Spending quality time with patients improves their outcomes and helps me - they have much advice and experience to share. Once in a while, after a treatment session, I will ask a patient, "how much do I owe you for today?"