Are masks required at CoachAmyPT?
Effective October 31, 2022, a mask is optional but encouraged in the CoachAmyPT clinic, especially for patients with health and exposure concerns. If you are unwell, don't hesitate to contact your therapist and reschedule your appointment. Thank you for helping to keep everyone safe and healthy!
How Much Does Physical Therapy Cost?
You are worth it!
Your ability to move and function in the future is worth the time and money spent with a movement specialist like Coach Amy.
Quality 1:1 Care
CoachAmyPT is a physical therapist-owned practice specializing in orthopedic outpatient and sports performance and does not employ students, assistants, trainers, techs, or aids.
To provide you with the maximum quality of care, Coach Amy evaluates and treats all patients 1:1, never overlapping or double-booking.
Treatment sessions and evaluations cost $60 to $250 or more, depending on several factors. Read the information below to help you plan financially.
Self-Pay Physical Therapy, Wellness, and Sports Performance Patients
CoachAmyPT provides transparent flat-rate pricing for all self-pay services. You can find these on the Schedule Appointment page on the website coachamypt.com.
The total cost of your care throughout treatment depends on the number of visits needed to achieve your health and wellness goals. This number varies and is unique to each patient, but we will provide a good-faith estimate upon request after an initial evaluation is completed.
Insurance Patients
CoachAmyPT is in network exclusively with Blue KC and will submit service charges on your behalf. Blue will adjust these based on in-network rates and apply them to your deductible. Network rates vary and depend upon your plan.
Your insurance is a contract between you, your employer, and your insurance company. Contact your insurance company if you have questions about your bill, your plan, and whether you've met your deductible.
Physical Therapy is an Investment in You.
We know there is a lot of competition for your time and money regarding health and wellness, and we hope this helps you budget and plan for success.
Strength Class with Coach Amy
Coach Amy’s “Rewire your Run” class is a hit, so we are adding another session this October.
The “Rewire your Run” class includes a combination of neuromuscular drills, Pilates-style mat work, and functional exercises specific to running. We move slowly and intentionally in this class with internal and external resistance (bands, weights).
Moves are geared toward particular muscle groups and neuromuscular patterns specific to running but are also beneficial to non-runners.
You will walk like a penguin, crawl like a bear, and kick like a donkey.
Our focus is on quality and accurate motion that builds strength and stability safely and productively.
Thursday nights 6:00-6:45 PM at the CoachAmyPT clinic. There are a few spots open, but space is limited. Registration for the October 2022 Session is available now.
Do I need a Doctor Referral for Physical Therapy?
Missouri and Kansas approved direct access to physical therapists, meaning you do not need a doctor to seek or receive physical therapy. You have direct access to Coach Amy. Direct access streamlines your access to physical therapy, decreases wait times, and, in most situations, decreases the overall cost by eliminating a visit to your primary care doctor. Still, suppose you have a doctor's referral or imaging results with a specific diagnosis. In that case, Coach Amy must evaluate you to ensure her clinical findings are consistent with that diagnosis.
What is a Physical Therapy Evaluation and Diagnosis?
A physical therapy evaluation aims to diagnose function or movement-related problems that underlie your symptoms.
Coach Amy will establish a functional diagnosis for you; this is not a medical diagnosis.
A physical therapy diagnosis is a functional diagnosis.
After evaluating a patient with foot pain, Coach Amy may determine that symptoms are consistent with plantar fasciitis, tarsal tunnel, or tendonitis, for example.
As a part of the diagnostic process, Coach Amy will:
obtain a relevant history
perform a systems review
administer specific tests and measures
Your functional diagnosis will guide Coach Amy in deciding the most appropriate intervention strategy. Even if the diagnostic process does not lead to a specific disorder, syndrome, or category, treatment is still possible. Coach Amy will design a custom treatment plan to alleviate symptoms, impairments, and activity limitations.
Coach Amy may refer you to other healthcare professionals for additional testing, such as imaging studies, or if she determines that your diagnosis is outside her scope of practice or expertise.
You do not need to go to a doctor when you seek physical therapy. Even if you have a doctor's referral or imaging results with a specific diagnosis, Coach Amy must evaluate you and determine whether her clinical findings are consistent with that diagnosis.
How to Treat an Acute Injury
“Texts from patients with acute injury are commonplace. The number one question is, “what should I do?” This is followed by, “should I make an appointment?” and “can I still run, play tennis, etc.?””
At the onset of a new injury, it is normal to feel fear and confusion about what to do next. Mild injuries can resolve quickly with early intervention and proper treatment. Follow Coach Amy's tips to prevent further damage, chronic injury, and pain.
Stage 1 (first 24 hours)
Rest
Rest from activity is the priority during stage 1.
Is there noticeable swelling and pain?
Ice the area for 20 min with at least 20 min between icing sessions.
Repeat icing throughout the day as needed.
If the injury is in a limb, prop it up on pillows so it is above your heart.
You can also apply compression for support and to help reduce swelling. Remove compression if you lose sensation, experience numbness or tingling, or the skin turns blue or white.
Avoid over-the-counter anti-inflammatory medications.
If pain is minimal and no swelling is present, skip to Stage 2.
Stage 2 (24-48 hours)
Painfree Movement
The goal during stage 2 is to promote healing by decreasing inflammation and improving blood flow.
Avoid bed rest; movement helps the healing process.
Move within a pain-free range.
Refrain from activities that cause pain greater than a 3/10 on the pain scale (see below).
Apply deep heat.
Try an ice-cup massage to help control pain if needed.
Avoid over-the-counter anti-inflammatory medications.
Coach Amy's favorite treatment at this stage is the application of deep heat for 20 minutes, in particular, EPSOM soaks.
Stage 3 (72+ Hours)
Return to activity as Tolerated
Stage 3 promotes healing with deep heat, movement, and a return to activity as tolerated.
Consider dry needling and Active Release Technique (ART). These treatments promote healing at this stage.
Dry needling is the most effective anti-inflammatory.
Gradually return to activities using pain as your guide. If your pain exceeds 3/10 with a movement or exercise, stop. See the pain scale below.
Make an appointment with your physical therapist or other health care provider for an evaluation if symptoms persist.
Pain scale:
It can be difficult to rate your pain. In physical therapy, we like to use the pain scale. [0=no pain, 10=emergency room pain]. If you have to limp or use poor biomechanics to move, your pain is likely higher than a 3/10.
Things not to do:
Avoid the temptation to stretch; refrain from massage and massage guns. These can provide temporary relief but, at the same time, cause more damage, especially in the acute phase of an injury when connective tissue tears are likely.
When Emergency Intervention is needed:
The following musculoskeletal symptoms are a medical emergency.
sudden, persistent weakness
inability to support weight on a limb
severe, uncontrolled pain or swelling
numbness and tingling in both legs
lack of bowel or bladder control or difficulty urinating
Seek immediate medical attention if you are experiencing chest pain or in case of a severe fall or accident, as internal injuries may be present.
Use Coach Amy's tips to help negotiate your acute musculoskeletal injury and prevent further damage, chronic injury, and pain. Schedule an appointment if symptoms do not resolve.
Missouri and Kansas approved direct access to physical therapists, meaning you do not need to go to a doctor when you seek physical therapy.
How to Treat Injury with Deep Heat
What is Deep Heat?
I recommend deep heat for most chronic pain and late-stage acute injury cases (48-72+ hours) to treat inflammation and pain and improve blood flow. Moist heat penetrates deeper than dry heat like an electric heating pad and can reach injured structures below skin level.
Types of Moist Heat
Moist hot packs are available at drug stores and online, but my favorite method is a 20-minute soak in a hot water bath with magnesium sulfate, known as Epsom "salts."
Dissolve 2 cups of 100% magnesium sulfate per gallon of hot water (100-102 degrees). Check your owner's manual before adding to hot tubs and jetted tubs.
Currently, no clinical trials support that magnesium sulfates can penetrate the skin; however, there is plenty of circumstantial evidence from athletes and patients that it helps!
“But Coach Amy, I hate soaking in a tub.” If you don't like soaking your whole body in a tub but want to treat your ankle/foot or lower leg, try a foot bath or a large bucket.
Caution
Take care if you have sensitive skin before using Epsom Salts. Soak a small body part in the magnesium sulfate bath first to see if you get an adverse reaction. A hot water soak is quite beneficial even without the Epsom.
Contraindications to Soaking in a Hot Tub or Bath
Diabetes
Rash
Low blood pressure
Blood vessel disorders
Rheumatoid Arthritis or Gout
Heart disease
Pregnancy
Seek advice from your healthcare provider if you are unsure whether soaking in a hot bath is safe.
If symptoms persist and impact your ability to function, schedule an appointment with Coach Amy. Missouri and Kansas approved direct access to physical therapists, meaning you do not need to go to a doctor when you seek physical therapy.
The application of heat is all about controlling inflammation. To learn more about inflammation and its impact on injury, health, and pain, check out Coach Amy’s three-part series:
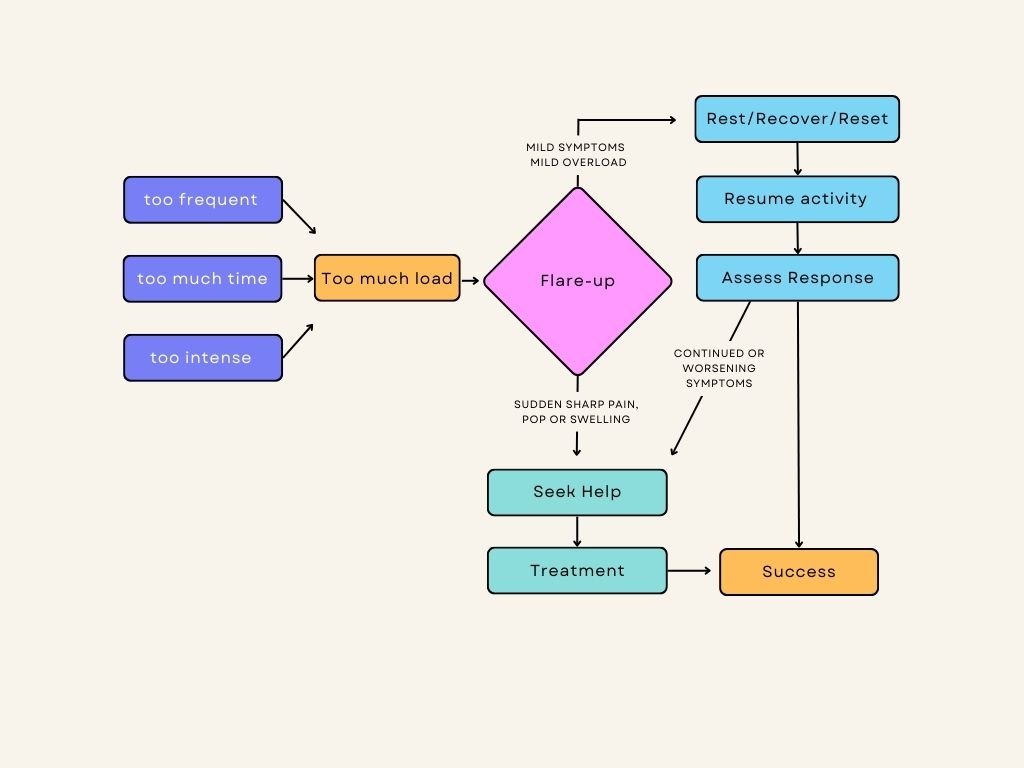
Ask Coach Amy - What's a Flare-up?
I was doing great, and now I am in pain again. What happened? Am I ever going to get better? - anonymous patient
It is common to suffer a setback when rehabilitating an injury. I refer to these as flare-ups. They tend to happen when you start feeling good enough to resume more activity and when you no longer have a constant reminder of your injury.
What is a flare-up, and what causes them?
A return of your original symptoms is a sign of a flare-up; this might be pain, less range of motion, or decreased strength. Flare-ups typically occur when resuming activity "too much, too soon."
Let's look at three "flare-up" scenarios in a tennis player recovering from lateral epicondylitis (tennis elbow) - an injury to a tendon in the elbow. For the first time in months, she can grip her Yeti water bottle and swing her racquet without pain.
Scenario I - Too intense (resistance or speed)
She returned to strength class and used the same amount of resistance she did before her injury.
Scenario II - Too long
She played a competitive 90-minute tennis match.
Scenario III - Too frequent
She played tennis five days in a row: a private lesson, a group lesson, and three friendly matches.
It is not uncommon to see a patient simultaneously make all three mistakes. In each example, this patient resumed her previous activity level too soon. There was too much load on her tendon, resulting in a flare-up.
How do I avoid flare-ups?
Return to activities gradually to allow for adaptation to new loads. What does this mean?
Return to one activity at a time to prevent overloading and to assess which exercise or motion is most likely responsible for the flare-up. For example, the tennis player could choose between strength class or tennis until her tendon is stronger.
Return to activities with at least one day of rest/recovery between bouts to provide adequate time for the injured area to adapt to new loads and assess your body's response. For example, the tennis player could resume tennis lessons or matches three days per week with a rest day between each bout.
Return to activities with low intensity, gradually increasing as tolerated. The tennis player in our example could resume easy play, friendly non-competitive matches, or tennis lessons starting with 30 minutes at a time.
Does a flare-up mean the injury is back or worse, that it will never get better?
Not necessarily. If the error in return to activity is not prolonged or excessive and the flare-up is mild (less than 3/10 on the pain scale), you're unlikely to be re-injured.
Sometimes it is hard to rate your flare-up severity on the pain scale, especially if you are worried about it. Patients often wonder if their flare-up is in their heads. And sometimes, it is!
Worry and concern can create phantom injury pains and inflate a mild symptom into the scary red zone. Follow the steps outlined in the flowchart below to address a flare-up.
Who gets flare-ups?
Flare-ups can happen to anyone, including professional athletes, coaches, and even physical therapists! We used a tennis player in our example, but the rules apply to most injuries we see in orthopedic physical therapy.
For example, our flare-up example also applies to a mom with pain in her shoulder when she reaches back in the car to grab her purse. It also applies to a patient with back pain when she unloads the dishwasher and the triathlete that experiences numbness after 20 min on the bike.
What should I do in the event of a flare-up?
Take a few days to rest, recover and reset. Treat symptoms, reset expectations, and resume activities gradually. Schedule an assessment and treatment with your physical therapist if symptoms persist or worsen after a week.
If the return to activity is excessive or the flare-up is severe, you might need more time to recover and some physical therapy to get over the hump.
If you suffered sudden, sharp pain, felt a pop, or sudden loss of stability, you may have re-injured the structure or damaged a new one. See your physical therapist or other direct access health care provider as soon as possible.
Flare-up Take Aways
Flare-ups are normal and happen to everyone.
Take steps to avoid flare-ups.
Rest, recover and reset when a flare occurs.
Seek help if needed.
Need help?
CoachAmyPT can help you recover from your flare-ups!
Wake Up Sleepy Glutes
Strong, healthy glutes are essential for running; they are the primary driver and power source. Yet, sometimes despite their good health and adequate strength, they fail to perform. The main culprits are sleepy glute muscles and an unstable platform. In a two-part series, How to Fire Up Your Glutes, Coach Amy provides a guide to overcoming these issues and getting the most out of your running glutes. In Part I, she explains how glutes can fall asleep on the job and how to wake them up.
Running with Coach Amy and the Roadrunners of Kansas City
Running is safer and more fun with a group! Join Roadrunners of Kansas City for supported group runs this spring on Saturdays at 7 AM for only $25 a month. Details are on the Roadrunners of Kansas City website. Click on the button below to learn more.